According to the Canadian Mental Health Association, 1 in 5 Canadians will experience a mental health issue in any given year and by the age of 40, there is a 50% chance you will either have or have had a mental illness.
Anxiety affects about 5% of Canadians with at least 8% of us experiencing major depression at some point in our lives with suicide representing a leading cause of death in Canadians aged 15-44.
Medications for these disorders are among the most commonly prescribed in Canada.
Mental Health is no joke.
Today’s article will not only introduce you to a more personal side of me, but will also explore nutrition’s role in the prevention and management of mental illness.
My Story
Today I am choosing honour my dearly departed friend Josh with an exploration of the evidence connecting nutrition mental health.
Josh, who I’d known since we were both kids, lost his battle with mental illness in February 15′.
At the time of his passing he was pursuing a Masters of Science and specifically examining the effect of antioxidant supplementation for symptom management in those taking anti-psychotic medications and has since been posthumously awarded with a MSc for his work.
Although I rarely discuss such intense personal matters, sharing his story and keeping his memory alive are important to me and today’s article serves as a small tribute to him, while also hopefully opening up the discussion on the connection between nutrition and mental illness.
Let’s get started.
Nutrition & Depression – Observational Evidence
I don’t think it should particularly surprise anyone to hear that those with higher intakes of fruits, veggies, whole grains and fish tend to have a lower depression risk than those with lower intakes of these foods.
Case in point, those who strongly follow a Mediterranean diet pattern were better protected against depression than those who just follow it moderately, especially with advancing age.
Another observational study linked anti-inflammatory diets with a reduced depression risk.
Although it isn’t necessarily the best descriptor of a dietary pattern, take a look at one of my previous articles here to get a better understanding of the foods that may be considered anti or pro-inflammatory.
Generally nutrient-poor diets are also associated with differences in physical features of the brain.
An imaging study found that those with poorer diets tended to have less left hippocampus tissue.
For those that may not know, the hippocampus is associated mostly with memory.
The association between nutrition and mental health is not exclusive to adults either.
In one study, diets that the authors identified as “good-quality” were associated with better mental health in children and adolescents. But what is a good quality diet?
An observational depression risk study out of China found that dietary patterns rich in red or processed meat, refined grains, high fat dairy products and paired with low fruit and vegetable intake, were associated with an increased depression risk.
In fact, “lower quality” diets consumed during pregnancy were found to be associated with a higher risk of a child dealing with either externalizing or internalizing disorders ( a type of behavioural issue).
Although I’ve presented observational rather than causal data in this first section, we can still see right off the bat that there is an intriguing link that exists between overall dietary patterns and depression risk in particular.
Nutrition & Mental Health – Experimental Evidence
What happens when you take people living with, or at risk of, mental illnesses ( such as depression) and use healthier eating as an intervention to improve outcomes?
Well, A 2013 trial out of the BMC journal found that a Mediterranean diet supplemented with tree nuts reduced the likelihood that men and women with type 2 diabetes would be diagnosed with depression.
In 2017, a BMC journal paper shared the results of a noteworthy randomized controlled trial known as the “SMILES” trial.
The Smiles Trial – An Overview
Participants: Individuals living with moderate to severe depression ( most using some form of other therapy as well)
Intervention: 12 week period. Dietary intervention ( 7 visits with a dietitian) vs Control ( 7 visits with a social support group).
Outcome Of Interest: Depression symptoms as measured by the well recognized MADRS scale
Results: Dietary intervention proved significantly superior in improving outcome of interest.
Conclusion: Dietary intervention with the assistance of a dietitian has the potential to help reduce symptoms in those already diagnosed with moderate to severe depression.
Translation?
Working with a dietitian to improve your dietary pattern is a worthwhile endeavour that has significant implications for improving both your general and mental health.
Flavonoids
Generally speaking, when you follow a strong, diverse dietary pattern, you get plenty of antioxidants.
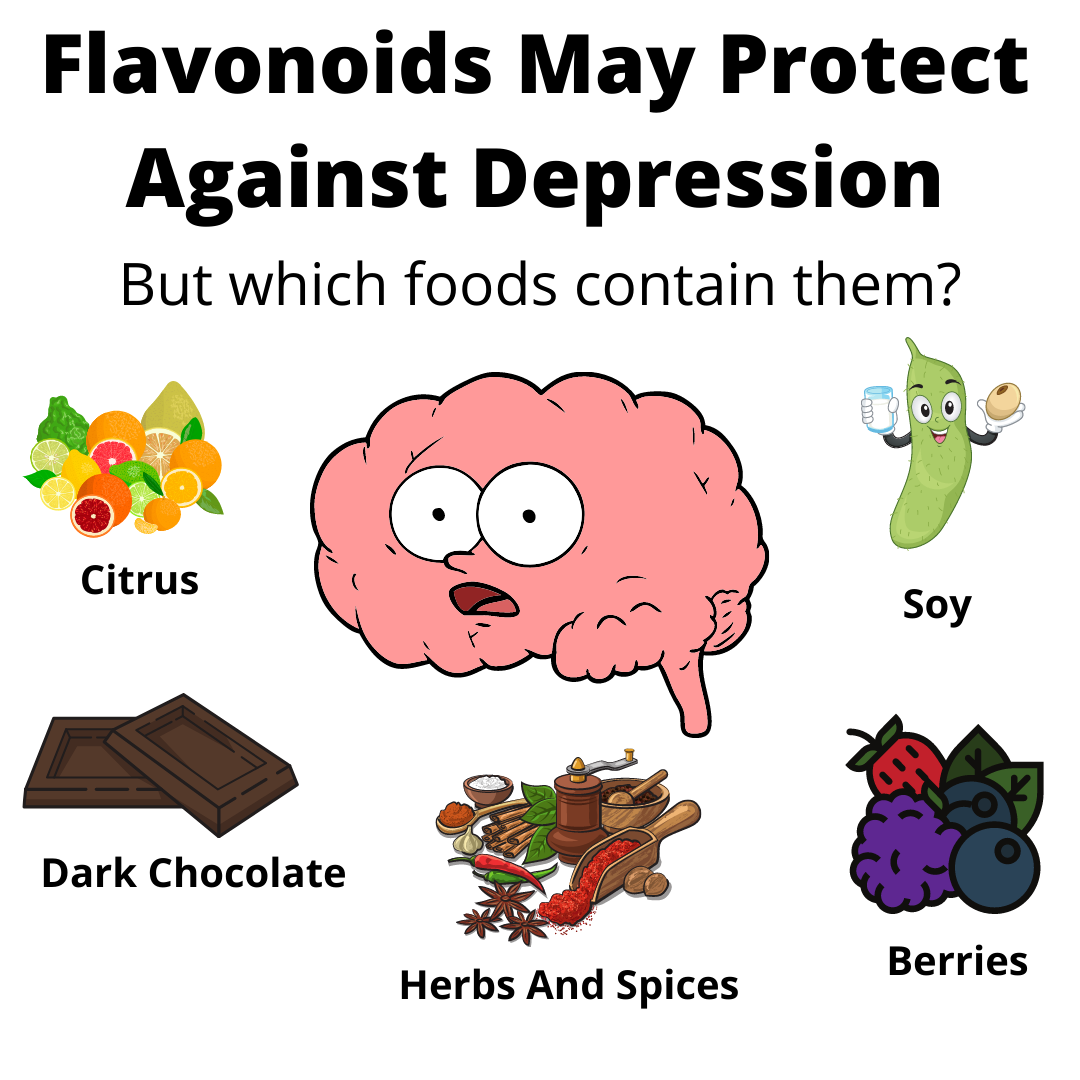
For that reason, it comes as no surprise that this 2016 AJCN paper found that flavonoids ( a family of phytochemicals with antioxidant capabilities) may be protective against depression in older women.
Studies suggest flavonoids have a role to play in preventing neuroinflammation ( ie – inflammation/damage of brain cells) and they are being increasingly considered as an alternative management modality in the world of mental health.
Provided here is a useful, if not aesthetic, chart that outlines some of the richest sources of dietary flavonoids.
Zinc, Magnesium, Selenium
There is some limited evidence examining the role that zinc, selenium and magnesium play in modulating depression risk and symptoms.
Magnesium in particular is a nutrient of interest for the simple reason it tends to be under-consumed in Canada.
I am including this sub-heading with minimal context as a great opportunity to remind everyone to eat a wider variety of nuts, seeds and legumes.
These are healthy foods that we don’t get enough of, that contain plenty of zinc and magnesium, and are included in great supply in the healthy dietary patterns ( such as the Mediterranean diet) that tend to be associated with a lower depression risk.
Final Thoughts
Today’s blog is wholly dedicated to my dear and departed friend Josh.
It is obviously just a small taste of this vast field of study, but hopefully it provided valuable insights none the less.
Until next time,
#LetsTalk
Andy De Santis RD MPH
Bonus Content